+918048034404
This is your website preview.
Currently it only shows your basic business info. Start adding relevant business details such as description, images and products or services to gain your customers attention by using Boost 360 android app / iOS App / web portal.
'Discover expert insights on living donor liver...
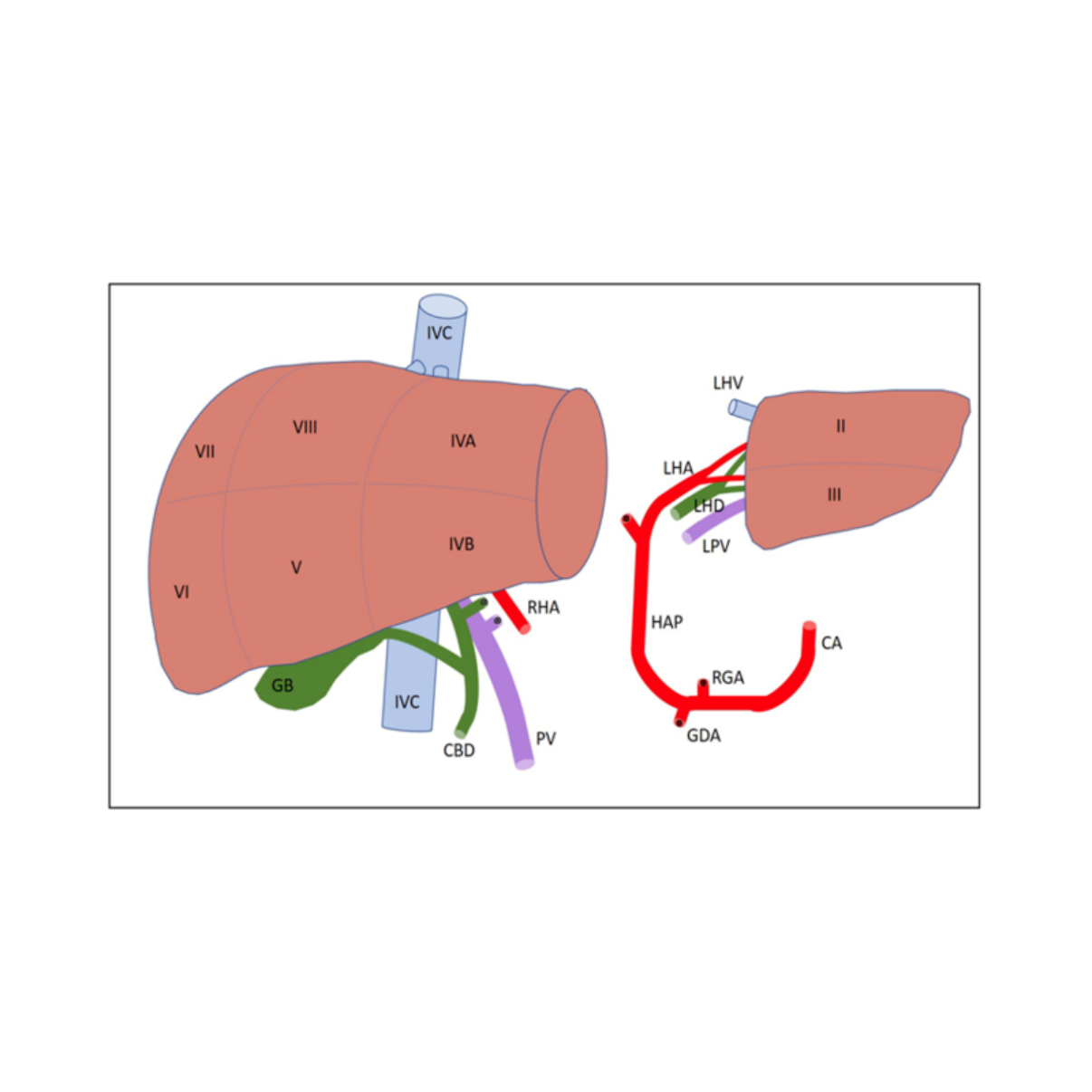
'Discover expert insights on living donor liver transplant, including donor selection, graft sizing, and pairing for successful outcomes. Dr. Chetan Kalal, the first DM Hepatologist in Maharashtra, offers specialized guidance for optimal liver transplant success.' Living Donor Liver Transplant: Donor Selection and Donor-Recipient Pairing 1. Donor Evaluation: Living donor hepatectomy is a complex and high-risk procedure, unlike any other surgery since it involves healthy individuals donating part of their liver. The donor’s well-being is the priority, and their thorough evaluation is essential to ensure safety. This process starts with a detailed medical history and physical examination to identify any contraindications, such as chronic liver disease, malignancy, cardiovascular conditions, diabetes, obesity (BMI >30), and substance abuse. Blood tests, imaging (CT, MRI), and, if needed, a liver biopsy help assess liver health and suitability for donation. A multidisciplinary team, including transplant surgeons, hepatologists, social workers, and psychologists, reviews the donor’s evaluation to ensure the risks are well understood and that donation is voluntary. 2. Graft Selection: The liver consists of eight segments, each with distinct allocations for different patient types. The left lateral section (segments II and III) is typically reserved for pediatric recipients, while the right lobe (segments V-VIII) is best suited for adults or larger pediatric recipients. Imaging studies like CT or MRI are used to evaluate the liver’s size, abnormalities, and anatomy. A detailed assessment ensures the graft’s size and health align with the recipient’s needs. The graft-to-recipient weight ratio (GRWR) is critical; a ratio greater than 0.8% is deemed safe for adult recipients, while smaller ratios may increase the risk of complications like small-for-size syndrome (SFSS). 3. Recipient Considerations: Recipient selection is guided by several factors, including graft volume and GRWR. Larger grafts, such as right lobe transplants, are often preferred for heavier recipients or those with severe portal hypertension. For children or smaller adults, left lobe grafts are generally used. Portal hypertension, a common issue in liver transplant candidates, is managed through various techniques to optimize graft function and reduce complications. 4. Donor and Recipient Outcomes: While the donor’s risks include bleeding, infection, and biliary complications, the overall morbidity rate is between 8% to 40%, with mortality rates at 0.2% to 0.5%. Right hepatectomy typically carries higher risks due to its complexity. For recipients, risks include biliary and vascular complications, especially with living donor grafts, which may face higher rates of hepatic artery thrombosis (HAT) and portal vein thrombosis compared to deceased donor transplants. However, with appropriate graft selection and careful surgical techniques, outcomes for living donor liver transplants are highly favorable. 5. Pediatric and Split Liver Grafts: Pediatric liver grafts are typically allocated to pediatric recipients, but in certain situations, they may be offered to adult recipients with careful consideration of graft size. Split liver transplantation, where a single liver is divided into sections for both pediatric and adult recipients, helps address organ shortages. Both in situ and ex vivo techniques are used to split the liver, depending on donor conditions and surgical expertise. These methods aim to reduce cold ischemia time and improve graft viability. Living donor liver transplantation, when carefully managed, provides life-saving opportunities for both donors and recipients, ensuring successful outcomes with meticulous evaluation and precise matching of grafts and recipients.

