+918048034404
This is your website preview.
Currently it only shows your basic business info. Start adding relevant business details such as description, images and products or services to gain your customers attention by using Boost 360 android app / iOS App / web portal.
earn about liver disease severity, risk assessm...
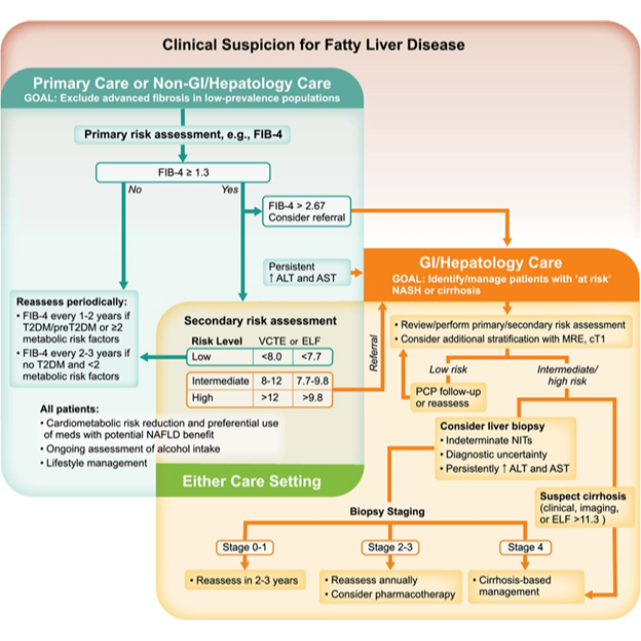
earn about liver disease severity, risk assessment tools like FIB-4, VCTE, and ELF, and when to consider liver biopsy for patients with MASLD. Ensure timely diagnosis and optimal care. Understanding Liver Disease Severity and Risk Assessment in MASLD Liver disease severity plays a critical role in determining a patient's prognosis and guiding treatment decisions. For patients with Metabolic Associated Steatotic Liver Disease (MASLD), identifying the stage of the disease can significantly impact outcomes. This article explores why establishing liver disease severity is crucial, the tools used for primary and secondary risk assessments, and when more invasive testing like liver biopsy may be necessary. 1. The Importance of Establishing Liver Disease Severity Identifying the severity of liver disease is essential for several key reasons: • Guiding Treatment Decisions: Understanding the stage of liver fibrosis (scarring) helps healthcare providers decide whether immediate intervention is needed or if ongoing monitoring is sufficient. • Predicting Long-Term Outcomes: Early detection of advanced liver damage can prevent serious complications such as cirrhosis, liver failure, and liver-related mortality. Advanced fibrosis or cirrhosis increases the risk of liver-related health events, which is why timely identification is vital. • Risk Stratification: Early assessment enables healthcare providers to stratify patients according to risk, allowing for more personalized care and management strategies. This can be particularly valuable in preventing disease progression to liver cirrhosis. In the clinical case provided, the patient’s initial FIB-4 score of 1.51 and elevated liver enzymes (AST 62, ALT 72) indicate the need for further evaluation through secondary risk assessments. By detecting liver disease severity early, clinicians can initiate the appropriate course of action. 2. Primary Risk Assessment of Fatty Liver Disease Primary risk assessment aims to identify patients who may have advanced liver disease. The FIB-4 score is a widely used tool that is simple to calculate and well-validated for identifying the likelihood of advanced liver fibrosis. It takes into account a patient’s age, AST, ALT, and platelet count. Key Takeaways from FIB-4: • FIB-4 < 1.3: This indicates a low risk of advanced fibrosis. Patients with a score below 1.3 can usually be safely monitored in the primary care setting. These patients should be reassessed every 1-2 years, particularly if they have risk factors like Type 2 Diabetes (T2D), prediabetes, or metabolic issues like high BMI, dyslipidemia, or hypertension. • FIB-4 ≥ 1.3: For patients with a score of 1.3 or greater, secondary risk assessment is needed to further evaluate the stage of liver disease. Secondary tests, such as vibration-controlled transient elastography (VCTE) or Enhanced Liver Fibrosis (ELF), are used to assess the degree of liver fibrosis more accurately. The FIB-4 score is a valuable tool for excluding advanced fibrosis, but it is just one part of the risk stratification process. Once a score above 1.3 is reached, further assessment using more sophisticated methods, such as VCTE or ELF, is necessary. 3. Secondary Risk Assessment Tools for Liver Disease For patients with a FIB-4 score greater than 1.3, secondary risk assessment is essential. The most commonly used tools for this purpose are: • VCTE (Vibration-Controlled Transient Elastography): This non-invasive test measures liver stiffness (which correlates with fibrosis) and steatosis (fat content in the liver). It provides a comprehensive evaluation of liver health, with results expressed in kPa (liver stiffness) and dB/m (Controlled Attenuation Parameter, or CAP, which indicates steatosis). o Fibrosis Assessment: Liver stiffness measurement is reported in kPa. Higher kPa values indicate more severe fibrosis. o Steatosis Grading: The CAP score helps categorize the degree of fat accumulation in the liver: S1 (Grade 1): 11-33% of the liver with fat content (CAP 238-260 dB/m) S2 (Grade 2): 34-66% fat content (CAP 260-290 dB/m) S3 (Grade 3): More than 67% of the liver affected (CAP >290 dB/m) • ELF (Enhanced Liver Fibrosis): This blood test measures biomarkers associated with liver fibrosis. It is especially useful for patients who may not have easy access to VCTE or for those with central obesity or implanted devices that interfere with VCTE measurements. Patients with low-risk results from these tests (VCTE < 8 kPa or ELF < 7.7) can be monitored in primary care settings. However, patients in the intermediate or high-risk groups (e.g., VCTE 8-12 kPa or ELF 7.7-9.8) may require additional evaluation, such as MRI-based testing, to further assess their liver condition. 4. When to Consider Liver Biopsy In certain circumstances, despite using non-invasive testing (NIT), liver biopsy may still be necessary: • High Suspected Risk of Cirrhosis: If a patient is at high risk of cirrhosis based on clinical suspicion, liver biopsy may provide definitive confirmation. • Indeterminate NIT Results: When non-invasive tests yield unclear results, liver biopsy can provide more conclusive information. • Diagnostic Uncertainty: In cases of suspected comorbidities affecting liver health, liver biopsy helps clarify the exact diagnosis. • Persistently Elevated Liver Enzymes: If ALT and AST remain elevated for over six months, liver biopsy may be required to assess the extent of liver damage. Conclusion Liver disease severity assessment is a fundamental aspect of managing MASLD and other liver conditions. Using tools like FIB-4 and secondary assessments like VCTE or ELF can provide an accurate picture of liver fibrosis and help guide treatment decisions. For patients with indeterminate or intermediate results, advanced imaging tests and, in some cases, liver biopsy may be necessary. Early and accurate assessment allows for appropriate interventions, reducing the risk of disease progression and improving patient outcomes. By utilizing validated tools for both primary and secondary risk assessment, healthcare providers can ensure timely management, optimizing care for patients with fatty liver disease.

