+918048034404
This is your website preview.
Currently it only shows your basic business info. Start adding relevant business details such as description, images and products or services to gain your customers attention by using Boost 360 android app / iOS App / web portal.
Learn about managing portal vein thrombosis in ...
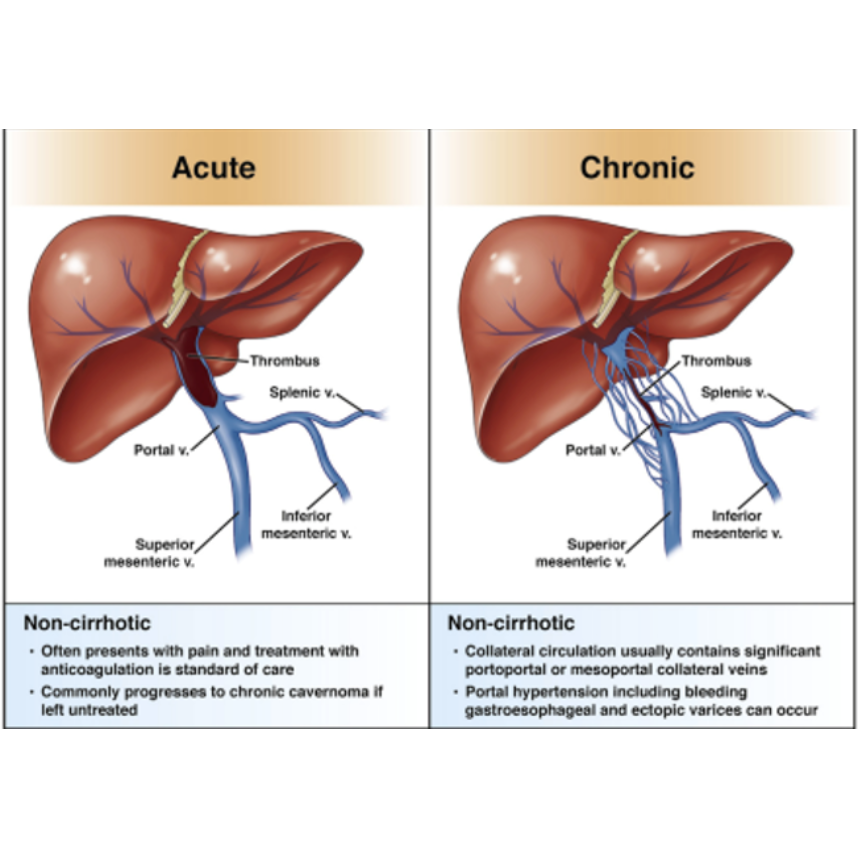
Learn about managing portal vein thrombosis in non-cirrhotic patients, including anticoagulation, infection, mesenteric ischemia, and chronic PVT care. Management of Portal Vein Thrombosis (PVT) in Non-Cirrhotic Patients: Immediate Goals and Treatment Approach Immediate Goals: • Prevent thrombus propagation • Promote vessel recanalization In general, unless there is a high bleeding risk, patients with portal vein thrombosis (PVT) without cirrhosis should be initiated on systemic anticoagulation. The primary aims are to prevent intestinal ischemia, avoid thrombus extension, and reduce the risk of developing chronic PVT and its consequences, such as portal hypertension. ________________________________________ PVT with Mesenteric Ischemia An acutely life-threatening complication of PVT is mesenteric ischemia, caused by clot extension into the mesenteric veins. Clinical indicators include: • Acute abdomen (peritonitis, rebound tenderness) • Shock • Persistent lactic acidosis • High-grade radiographic signs of intestinal compromise Patients with suspected mesenteric ischemia should undergo emergent evaluation for exploratory laparotomy and potential resection of ischemic or necrotic bowel. Timely surgical intervention can be lifesaving. ________________________________________ PVT with Thrombophlebitis (Pylephlebitis) In non-cirrhotic PVT, another important consideration is superimposed infection — known as pylephlebitis. Key points: • Fever is present in up to 50% of cases. • Bacteremia occurs in up to 70% of patients. • Infections are often due to gut-derived organisms (gram-negative and anaerobic species). Management includes: • Initiation of broad-spectrum antimicrobials • Systemic anticoagulation to prevent further thrombus propagation Keywords: pylephlebitis management, infection in portal vein thrombosis ________________________________________ Management of Other PVTs in Non-Cirrhotic Patients For non-tumoral PVT (especially recent clots): • Systemic anticoagulation is the cornerstone of therapy. • Recanalization rates vary from 16% to 71% depending on clot burden, timing, and therapy. Anticoagulation Regimens: • Minimum 6 months of therapy is recommended if the underlying risk factor has resolved. • Patients with underlying thrombophilias often require lifelong anticoagulation. Preferred Anticoagulants: • Low Molecular Weight Heparin (LMWH) remains the most commonly used treatment in the acute setting. • Vitamin K antagonists (e.g., Warfarin) are also widely used. • Direct Oral Anticoagulants (DOACs) (e.g., rivaroxaban, apixaban) show promise and are increasingly prescribed for provoked PVTs or as maintenance therapy, though high-quality randomized data are still limited. Keywords: anticoagulation for portal vein thrombosis, LMWH for PVT, DOACs for portal vein thrombosis ________________________________________ Special Clinical Scenarios: A. Progression of Thrombus Despite Medical Therapy If there is thrombus progression and signs of imminent bowel infarction, urgent intervention is necessary: • Endovascular thrombolysis may be considered (including TIPS placement if needed). • Recanalization rates with thrombolysis can be as high as 90%. • Surgical intervention (bowel resection) remains critical in cases of established bowel necrosis. B. Chronic Non-Cirrhotic PVT Features of chronic PVT may include: • Ascites • Gastroesophageal varices • Splenomegaly Management Focus: • Primary prophylaxis (with non-selective beta-blockers or endoscopic variceal ligation) and secondary prophylaxis for variceal bleeding are recommended. • Note: These recommendations are largely extrapolated from studies in patients with cirrhosis. Role of Anticoagulation in Chronic PVT: • In patients with established portal collaterals and no underlying thrombophilia, anticoagulation or interventional therapy may offer limited benefit. • However, if a patient has a known potent thrombophilia (as in our case), lifelong anticoagulation remains indicated to prevent further thrombotic events. Keywords: chronic PVT management, portal hypertension in non-cirrhotic portal vein thrombosis ________________________________________ Conclusion The management of portal vein thrombosis in non-cirrhotic patients requires early diagnosis, careful risk stratification, and individualized treatment. Timely anticoagulation can promote recanalization, prevent intestinal ischemia, and reduce the risk of portal hypertension. Emergent intervention is crucial in cases of mesenteric ischemia or thrombus progression, while chronic PVT shifts the focus to managing complications of portal hypertension — with anticoagulation decisions guided by the presence of underlying thrombophilic conditions

